Dengue in Rohingya refugee/Forcibly Displaced Myanmar Nationals (FDMN) camps in Cox’s Bazar – Bangladesh
03 August 2022

Outbreak at a glance
Dengue is endemic in Bangladesh. As compared to the previous four years (2018 to 2021), the Rohingya refugee/Forcibly Displaced Myanmar Nationals (FDMN) [1] camps in Cox’s Bazar district, are experiencing an acute surge in dengue cases, that started at the end of May 2022 (epi week 22). As of 24 July (end of epi week 29), a total of 7687 confirmed cases and 6 deaths have been reported, with 93% (7178) of the cumulative number of cases being reported since the start of the surge at the end of May 2022 (Figure 1). A similar surge has not been observed in the larger Cox’s Bazar district outside of the Rohingya refugee/FDMN camps nor at the national level with case numbers and trends within expected levels of incidence for the same period. As dengue is recurrent in this part of the country, the population may be at risk of secondary infection, which puts them at higher risk for severe disease.
Description of the outbreak
From 1 January to 24 July 2022, a total of 7687 cases of dengue, confirmed by rapid diagnostic test (RDT), and six deaths (case fatality rate, 0.08%) have been reported from the Rohingya refugee/FDMN camps in Cox’s Bazar district, Ukhia Upazila and Teknaf Upazila (sub-districts), with the former sub-district being the most affected of the two. An acute surge of cases began during the week commencing 23 May (epi week 22), and peaked the week ending 26 June (epi week 25), with 93% (7178) of the cumulative number of cases being reported between 23 May and 24 July. A decreasing trend in reported dengue cases was observed following the peak when 1291 cases were reported in epi week 25; however case numbers remain high despite the decline: epi week 26 (1241), epi week 27 (1152), epi week 28 (962), epi week 29 (1000).
Cases of reported dengue in Rohingya refugee/FDMN camps are significantly higher as compared to similar periods over the past four years; 2018 (4 cases), 2019 (7 cases), 2020 (3 cases), and 2021 (1530 cases and 3 deaths with a surge from October to December) (Figure 1). However, at a national level and in the larger Cox’s Bazar district, case numbers have been within expected endemic levels of incidence; by comparison to the dengue case from the camps, the larger Cox’s Bazar district reported approximately 121 cases from 1 January to the end of June (epi week 27).
Camps located in Ukhia Upazila are predominantly affected by the outbreak. Camp 3 accounted for over 50% of all reported cases and Camps 4 and 1W each account for less than 10% of cases as of 24 July 2022. More than two-thirds of cases (67%) were among persons 15 years and older with males accounting for 60% of cases. The majority of cases (81%) were hemodynamically stable – not showing any warning signs for severe dengue syndrome (such as dengue hemorrhagic fever (DHF) or Dengue Shock syndrome (DSS)) nor having any coexisting conditions – while approximately 15% of cases were mild and required observation and admission to primary health facilities. Severe dengue with signs of DHF and DSS was observed in 0.3% of cases and required admission to Cox’s Bazar District Hospital located within the camp. Among patients admitted to the hospital, 1% required blood transfusion. Previous dengue infection was reported in 1% of current cases.
Serotyping results from 10 samples processed at the Institute of Epidemiology, Disease Control and Research (IEDCR) reference laboratory in the capital Dhaka identified DENV-3 (5 samples), DENV-2 (3 samples). Two samples had inconclusive results.
Dengue is endemic in Bangladesh with recurrent outbreaks. The Rohingya refugee/FDMN camps in Cox’s Bazar district previously experienced an acute dengue outbreak from October to December 2021 during which 1530 cases, including 3 deaths, were reported. Case numbers began to decline at the beginning of 2022, and by the end of February, the event was under control until the resurgence of cases in May 2022.
Figure 1. RDT-confirmed cases of dengue fever in Rohingya refugee/FDMN camps, Cox’s Bazar District, Bangladesh by notification date, 1 January 2018 to 24 July 2022*
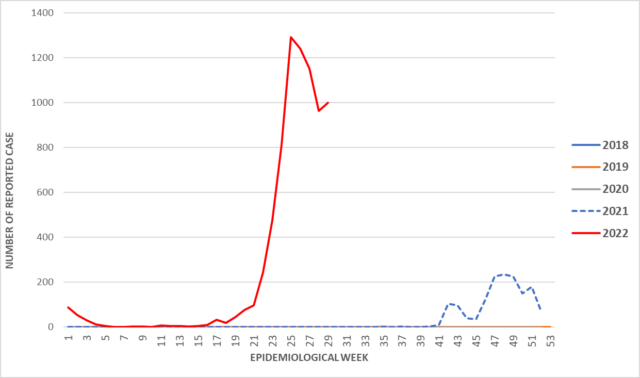
* Due to relatively low case numbers in 2018 to 2020, the curves for these years do not appear visible in the chart.
Epidemiology of the disease
Dengue is a viral infection transmitted to humans through the bite of infected mosquitoes and is found in tropical and sub-tropical climates worldwide, mostly in urban and semi-urban areas. The primary vectors that transmit the disease are Aedes aegypti mosquitoes and, to a lesser extent, Aedes albopictus.
Dengue virus (DENV) has four serotypes (DENV-1, DENV-2, DENV-3, DENV-4) and it is possible to be infected by each. Infection with one serotype provides long-term immunity to the homologous serotype but not to the other serotypes; sequential infections put people at greater risk for severe dengue. Many DENV infections produce only mild illness; over 80% of cases are asymptomatic. DENV can cause an acute flu-like illness.
There is no specific treatment for dengue; however, timely detection of cases, identifying any warning signs of severe dengue infection, and appropriate case management are key elements of care to prevent patient death and can lower fatality rates of severe infection to below 1%.
Occasional cases acquired overseas have been reported among individuals returning from an area with active dengue transmission, however, there is no conclusive evidence that there have been cases of dengue imported to Bangladesh.
Public health response
- The government of Bangladesh and the Health Sector established a multi-sector coordination group and organized meetings with technical partners to manage and coordinate the response.
- WHO supported the Bangladesh Ministry of Health and Family Welfare (MOHFW) to undertake an entomological survey of disease-causing mosquito vectors, including dengue vectors, within and around the camp areas.
- WHO led a risk assessment visit to the epicentre of the current outbreak (Camp 3) on 21 June 2022.
- WHO, through the Epidemiology Technical Working Group (TWG), continues to provide timely situational updates and guide on appropriate response.
- A dengue treatment protocol is being finalized by WHO to guide the detection and management of dengue cases including a referral pathway.
- WHO is currently finalizing the protocol on case detection and management.
- Cox’s District Referral Hospital and Médecins Sans Frontières (MSF) are managing severe cases. Other hospitals and isolation facilities at Primary Health Care Centers (PHC) or dedicated centers are also managing moderate and mild cases.
- The International Organization for Migration (IOM) PHC located in Camp 3 has dedicated ten isolation and six observation beds for dengue case management to cope with the surge.
- WHO has procured and is distributing RDT kits to health sector partners to ensure timely diagnosis across all sentinel facilities, some of which have isolation capacity.
- Multi-agency integrated response interventions including Water and Sanitation and Hygiene (WASH), environmental management, health, and Risk Communication and Community Engagements (RCCE) are currently being scaled up in the affected camps.
- WHO is supporting the transportation of NS1 antigen-positive dengue samples from different health facilities to the IEDCR Reference Laboratory in the capital Dhaka for PCR testing and serotyping.
WHO risk assessment
In August 2017, approximately 700,000 Rohingya nationals fled from Myanmar to Cox’s Bazar district, joining more than 200,000 Rohingya nationals already present, and settling into informal makeshift camps, marked by inadequate access to potable water or quality sanitation and challenging living conditions. The speed and magnitude of the influx exerted pressure on existing resources, strained healthcare services, water, and other social amenities. As a result, there have been high levels of global acute malnutrition (GAM) in children under five years; persistent transmission of acute watery diarrhoea (AWD); recurrent cholera epidemics that are transitioning into an endemic state; persistent diphtheria transmission since 2017; and occasional upsurges of measles, varicella, and skin infections.
Dengue virus has the potential to cause epidemics resulting in high morbidity and mortality. In Bangladesh, hospital capacity is limited and further increases in severe dengue cases may pose considerable challenges in case management. The Severe Acute Respiratory Infections Treatment Centres (SARI ITC) bed occupancy for COVID-19 admissions is 26% as of 26 June. As hospitals become burdened with people affected by the COVID-19 virus, the increase in hospitalized dengue cases may put undue strain on healthcare capacities.
Currently, the district of Cox’s Bazar can detect dengue using RDTs done in approximately 50 sentinel sites distributed across the 33 camps located in Ukhia and Teknaf Upazilas (sub-districts). There is currently no capacity for dengue virus serotyping at Cox’s Bazar Medical College Laboratory.
Cox’s Bazar previously experienced an acute dengue outbreak from October to December 2021. The current surge in dengue cases could be considered a continuation of last year’s transmission. As dengue is recurrent in this part of the country, the population may be at risk of a secondary infection that may lead to serious complications if not treated promptly and adequately.
Key challenges experienced during last year’s dengue upsurge included delays in the international procurement process for dengue RDT kits, the long process necessary for undertaking dengue virus serotype in the capital Dhaka given such capacity is not available in Cox’s Bazar, and weak vector surveillance and control.
In addition to the COVID-19 pandemic, other ongoing health events such as cholera/AWD (persistent low level of transmission) and diphtheria (persistent low level of transmission since September 2021) may pose additional challenges in response measures by competing for resources.
Population movement is now more pronounced in Bangladesh with the relaxation of COVID19-related movement restrictions. Cox’s Bazar does not have a direct international point of entry. However, it is close to the seaport in Chattogram and has a domestic airport that receives a large volume of local and international tourists and international humanitarian workers. These factors increase the possibility of international dengue introduction and spread.
WHO advice
The proximity of mosquito vector breeding sites to human habitation is a significant risk factor for dengue virus infection. Although dengue does not spread from human to human, Aedes species mosquitoes can become infected after biting dengue-infected individuals, thus creating a cycle of transmission capable of spreading dengue and leading to clusters of cases.
Vector control activities should focus on all areas where there is a risk of human-vector contact. WHO promotes a strategic approach known as Integrated Vector Management (IVM) to control mosquito vectors. IVM should be enhanced to remove potential breeding sites, reduce vector populations, and minimize individual exposure. This should involve vector control strategies for larvae and adult mosquitoes, including:
- Environmental management (i.e., source reduction by improving water storage practices) and eliminating stagnant pools of water.
- Larviciding non-potable waters using WHO prequalified larvicides
- Distribution of insecticide-treated nets (ITNs) in severely affected camps
- Provision of ITNs for fever/dengue inpatients in health facilities.
Indoor space spraying (fogging) is another approach for rapid containment of a dengue outbreak but may be challenging to deliver in densely populated areas within camps. Larvicidal prevention measures recommended by MOHFW and WHO are considered more impactful in breaking transmission compared to the targeting of adult mosquitoes with fogging and fumigation.
Personal protective measures during outdoor activities include the topical application of repellents to exposed skin or treatment of clothing, and the use of long sleeves shirts and pants. Indoor protection can include the use of household insecticide aerosol products or mosquito coils. Window and door screens, as well as air conditioning, can reduce the probability of mosquitoes entering the house. Insecticide-treated nets offer good protection to people against mosquito bites while sleeping during the day. Since Aedes mosquitoes are active at dawn and dusk, personal protective measures are recommended particularly at these times of day.
Entomological surveillance should be undertaken to assess the breeding potential of Aedes mosquitoes in containers as well as conducting insecticide resistance testing for vector control intervention.
Rapid detection of severe dengue cases and timely referrals to tertiary hospitals can reduce mortality. Case surveillance should continue to be enhanced in all affected areas and across the country. Where feasible, resources should be allocated to the strengthening of sample referral mechanism for the confirmation and sub-typing of the dengue virus.
WHO does not recommend that any general travel or trade restrictions be applied to Bangladesh based on the information available for this event
Further information
- WHO factsheet: Dengue and severe dengue
- WHO Q&A: Dengue and severe dengue
- WHO Health topics: Dengue and severe dengue
[1] The Government of Bangladesh refers to Rohingya as “Forcibly Displaced Myanmar Nationals”. The UN system refers to this population as Rohingya refugees, in line with the applicable international framework. In this document both terms are used, as appropriate, to refer to the same population.
Citable reference: World Health Organization (2 August 2022). Disease Outbreak News; Dengue in Rohingya refugee/Forcibly Displaced Myanmar Nationals (FDMN) camps in Cox’s Bazar, Bangladesh. Available at: https://www.who.int/emergencies/disease-outbreak-news/item/2022-DON401
Announcements
28 February 2025
Asian NGO Network on National Human Rights Institutions , CSO Working Group on Independent National Human Rights Institution (Burma/Myanmar)
Open letter: Removal of the membership of the dis-accredited Myanmar National Human Rights Commission from the Southeast Asia National Human Rights Institution Forum

Progressive Voice is a participatory rights-based policy research and advocacy organization rooted in civil society, that maintains strong networks and relationships with grassroots organizations and community-based organizations throughout Myanmar. It acts as a bridge to the international community and international policymakers by amplifying voices from the ground, and advocating for a rights-based policy narrative.