Myanmar women give birth in jungle as military lies in wait
21 July 2021

[JC/Al Jazeera]
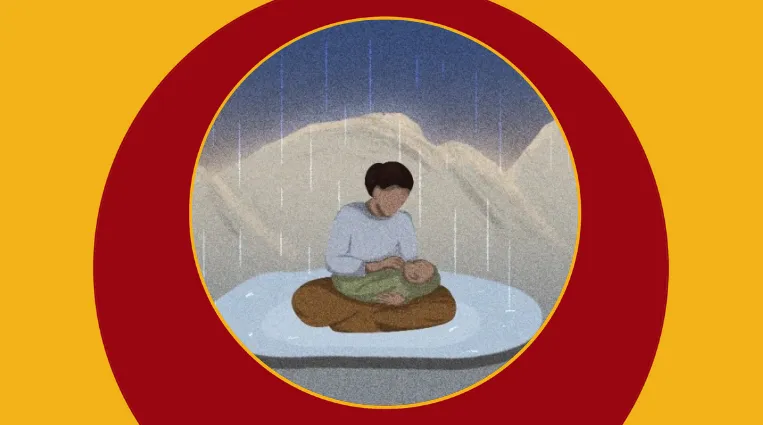
On a stormy night in June, Rosemary lay in the darkness of her home in a deserted village in Myanmar’s Mindat township, gripped by labour contractions as Mai Nightingale, a 25-year-old midwife, tried to stifle her cries.
“Only the two of us were left alone in the village. We closed all the doors and windows of the house and stayed quietly inside,” said Mai Nightingale. “When she felt pain, I put a blanket in her mouth because we feared that soldiers might hear her.” Like others interviewed for this article, Al Jazeera has used pseudonyms for Mai Nightingale and Rosemary for their safety.
“The situation didn’t favour delivering a baby,” said Mai Nightingale. “We saw Burmese soldiers walking towards our village but we couldn’t turn back because [Rosemary] was already exhausted.”
Rosemary’s husband did not dare accompany her for fear that, if seen, soldiers would mistake him for a member of a local armed group. Since a February 1 military coup, civilian defence forces, armed largely with hunting rifles and homemade weapons, have sprung up across the country to fight against the regime, and Mindat has been a hotspot of resistance since May.
In line with tactics the military has used for decades to quash an armed rebellion and terrorise the people, soldiers launched disproportionate attacks on Mindat including firing artillery, rocket-propelled grenades and machineguns into residential areas while imposing martial law, causing the town to empty, according to local media reports. Young men are particularly likely to be targeted.

[JC/Al Jazeera]
Rosemary delivered her baby shortly after the sound of soldiers had faded, and Mai Nightingale cut and tied the umbilical cord with a razor blade and some thread which, lacking other means of sterilisation, she boiled in water. Although Rosemary and her baby are healthy and unharmed, the circumstances of the birth highlight the increasing risks which mothers and newborns face amid an escalating humanitarian crisis.
Mai Nightingale and two other nurses interviewed by Al Jazeera, who are providing maternal and newborn healthcare to those displaced by armed conflict, say they are severely limited in their ability to safely deliver babies, and that physical insecurity further imperils pregnant women and newborns amid the continuing violence.
“The main health risks for pregnant women and newborn babies are their lives. They can die during labour or after because they have to run whenever soldiers get closer to where they are hiding,” said a nurse in Loikaw township, Kayah State who goes by the nickname Smile. “There is not enough medical equipment or medicine … Babies cannot get vaccinations or adequate shelter.”
Collapsing health system
Some 230,000 people have been newly displaced since the coup, according to United Nations estimates.
The military has not only attacked civilians but has also cut off food and water supplies to people affected by conflict, shelled displacement camps and churches of refuge, shot displaced people attempting to fetch rice from their villages, and burned food and medical relief supplies along with an ambulance.
Meanwhile, Myanmar’s health system has all but collapsed, leaving few options even for those women prepared to risk returning to their town or village to give birth or seek vaccinations or treatment for their babies.
Ongoing medical worker strikes amid a broader Civil Disobedience Movement have left government hospitals threadbare, while some health facilities have shut down altogether. The military has also repeatedly attacked healthcare professionals and facilities and occupied hospitals.
“My mother placed her hand on my cousin and prayed. By the grace of God, she successfully gave birth” – SMILE, MYANMAR NURSE
Alessandra Dentice, Myanmar representative ad interim with the UN Children’s Fund (UNICEF), told Al Jazeera that the vast majority of pregnant women displaced since the coup lack access to emergency obstetric care, while routine immunisations for children have “come to an almost complete halt”.
“Without urgent action, we estimate that annually 600,000 newborns will miss out on essential newborn care, creating serious risks for their survival and long-term wellbeing across the country,” she said, adding that about 950,000 children are also missing out on critical vaccination services.
In Mindat, Mai Nightingale has so far assisted three displaced women to deliver. Two of them, she said, had to keep moving in search of safe shelter in the days leading up to giving birth, causing them physical pain and possibly inducing their labour.

[JC/AL Jazeera]
Pregnant women in Kayah State, where an estimated 100,000 people have been displaced since early June, also face a perilous situation. On June 8, the UN special rapporteur for Myanmar warned of “mass deaths from starvation, disease and exposure” in Kayah due to military attacks and the blockage of food, water and medicine to those who fled to the forest.
Smile, a 24-year-old nurse, escaped her village in Loikaw township on June 11 with her cousin, who was in the throes of labour contractions while she fled. “Artillery fell near the rock where we were hiding. That day was [my cousin’s] due date but she couldn’t deliver … we had to escape to safety,” said Smile. “She had to carry heavy things while we were running.”
Recalling advice from her mother, also a nurse, Smile had grabbed a delivery kit with rubber gloves, forceps and scissors as she fled the village. “My mother told me that medical workers cannot stop even if the world is in chaos,” she said.
She and her mother rubbed down the equipment with spirits while her cousin’s husband built a bamboo and tarpaulin tent, under which they delivered her cousin’s baby. “My mother placed her hand on my cousin and prayed. By the grace of God, she successfully gave birth without [heavy] bleeding,” said Smile.
But tragedy has befallen some displaced mothers.
Little time to grieve
In Loikaw township, Khu Meh delivered twins at a local clinic on April 8. One was born dead; Khu Meh fled home with the other, a girl, in mid-May. “We travelled very far and moved from place to place, sometimes sleeping in the bushes,” she said. About three weeks later, the second twin died in the jungle while drinking milk at Khu Meh’s breast.
Some 40km (25 miles) north, in Shan State’s Pekon township, Mary fled her home in the last week of May, when she was more than seven months pregnant.
“The military was firing every night … we were very scared to sleep at home,” she said.
She sheltered in a church, but after it was shelled on June 6, she fled again, to a cornfield where she delivered her fifth child, a baby boy, under a bamboo and tarpaulin shelter with the help of a local midwife.
The next week brought endless rain, and Mary’s baby died suddenly. There was little time to grieve. Mary and her remaining children had to flee again a week later due to approaching soldiers.

[JC/AL Jazeera]
Maternal mortality was 250 deaths per 100,000 live births in 2017, while under-five mortality was 48 children per 100,000 live births.
Al Jazeera was unable to locate data on maternal and infant mortality among displaced populations in Myanmar since the coup.
Naw Winnie, a nurse from Demoso township, Kayah State who was herself displaced by fighting, is now volunteering with a local aid group in the mountainous area where she fled.
She told Al Jazeera that illness among young children is common. She has treated dozens of skin infections and cases of diarrhoea, and fears that health problems will only increase because of poor hygiene caused by factors including the scarcity of clean water and the lack of toilets.
The rainy season started in June, making sanitation more difficult and increasing the risk of catching a cold, flu, or mosquito-borne illnesses.
Naw Winnie is also looking after more than 10 pregnant women.
She had initially planned to send them to a temporary clinic near the foothills of the mountain, but the clinic’s volunteers and patients were forced to evacuate amid heavy fighting on June 16.
Now she is not sure what she will do.
One of the women, now more than five months pregnant, previously gave birth by Caesarean section, and Naw Winnie is concerned the woman could haemorrhage if she delivers vaginally, but it is simply too risky to perform a Caesarean section in the jungle.
“We don’t have access to safe and hygienic facilities or equipment to deliver babies,” she said. “If I assist in delivering a baby without hygienic facilities, it will put both mothers and babies in danger.”
Original Post: Al Jazeera News
Announcements
28 February 2025
Asian NGO Network on National Human Rights Institutions , CSO Working Group on Independent National Human Rights Institution (Burma/Myanmar)
Open letter: Removal of the membership of the dis-accredited Myanmar National Human Rights Commission from the Southeast Asia National Human Rights Institution Forum

Progressive Voice is a participatory rights-based policy research and advocacy organization rooted in civil society, that maintains strong networks and relationships with grassroots organizations and community-based organizations throughout Myanmar. It acts as a bridge to the international community and international policymakers by amplifying voices from the ground, and advocating for a rights-based policy narrative.